Aug 6
IUI or IVF? Choosing the Right Approach to Family Building
Kilian Melloy READ TIME: 1 MIN. SPONSORED
The family-building journey can be complex and involves many areas of a person’s, or a couple’s, life. The Prelude Network — North America’s largest and fastest growing network of fertility clinics — stands ready to offer the same respective and detailed-oriented attention to all who seek them out, regardless of whether they are partnered, single, queer, or straight. For LGBTQ+ families, however, that inclusive approach is especially important, because queer families are increasingly turning to assisted reproductive technologies to help them realize their dream of parenthood.
The complexities of the family-building journey can begin with the choice of whether to seek parenthood through IUI or IVF. Both are scientifically sound avenues to reproduction, and each has its own suite of considerations that might be more ideal to a family’s unique needs.
IUI, or intra-uterine insemination, involves stimulating the release of ova, or eggs, for a person with ovaries and then introducing sperm to the uterine cavity via a thin catheter, where fertilization can then take place.
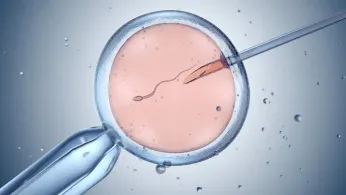
IVF, on the other hand, involves stimulating ovaries to produce multiple eggs, then removing them from the body before ovulation and uniting them with sperm cells under laboratory conditions. Resulting embryos are can be genetically tested before being implanted in the uterus of a prospective parent or a gestational surrogate.
Either method brings the three essentials for pregnancy together: Eggs, sperm, and a uterus, or womb, where an embryo can develop until childbirth occurs. Apart from the commonality of these required ingredients for new life, though, family-building can take many different routes — as many as there are family configurations.

Source: Prelude Fertility
Choosing between IUI and IVF can be relatively straightforward — or not. As Nurse Shana Puetz, Clinical Manager at Tennessee Fertility Institute explains, “It's usually a combination of factors on why you're going to choose one of the other, like medical history, personal preference of the patient, and financial considerations — because each treatment has a big difference in the overall cost picture.”
Puetz illustrates with the example of a couple in which both partners possess wombs and ovaries. At first glance, it might seem that procuring donor sperm and using IUI to achieve pregnancy for one of the members of the couple is the easiest and most straightforward path to parenthood — and that might be true in many cases. But sometimes, the picture is more complicated.
“Some patients are not going to have the option to pursue IUI,” Puetz notes. “For example, if you were a patient who had blocked fallopian tubes, that means that the sperm aren't going to be able to reach the egg. Even if we do all of the right things, we are not going to be able to have them meet — there's no way for us to get the sperm to the egg other than outside the body,” as with IVF.
As for the so-called “turkey baster” method, that’s something altogether different. “I think what people think of when they think of turkey baster is actually what we would call ICI, which is intra-cervical insemination,” Puetz clarifies. “Basically, you're putting the semen as far up in the vaginal canal as you can, to get it close to where the sperm can meet with an egg. What we're doing in an IUI is intrauterine. We're passing a very thin tube through the cervix up into the uterine cavity, and that's where we're placing the sperm.
“The other difference is the preparation for IUI,” Puetz continues. “There's a lot of debris in semen; there is a lot of dead sperm, there is a lot of extra fluid. When we do an IUI, that sperm sample will get processed by our andrology lab. I like to describe it as they're going to spin it down, they're going to clean it up, they're going to take our absolute best swimmers and concentrate them for us to put that sample up there, versus a ‘turkey baster’ method. And actually, most of that extra debris — liquid and dead sperm — are going to come right back out the vaginal canal, versus us putting them up into the uterus, so we've given the cleaned-up sperm a head start with IUI.”
For same-sex couples in which both individuals possess sperm, but not ova or wombs, the need for a gestational surrogate is a given. But here, too, different factors can influence a decision to proceed with IUI or opt for IVF instead. For instance: Like their cisgender and heterosexual peers, LGTBQ+ individuals with sperm might face fertility issues around sperm production or motility.
“Maybe there is just a small decrease in the amount of sperm, or maybe they don’t have as many swimmers as we would expect to see in terms of their mobility,” Puetz clarifies. “They can be a great patient to introduce IUI, just because we're removing the factor of the cervix and some of the cervical mucus, and we're bypassing that and going straight into the uterus, so we again give them that extra oomph to get there.”
But IUI might not be adequate if the number of sperm present are too low or their motility isn’t sufficient. Consider the story shared by reality TV star and former NFL football player Colton Underwood, who, together with his husband, contributed sperm for the fertilization of donated ova. Whereas his husband’s contribution contained the normal number of sperm cells, Underwood told the media, his own contribution held only a few sperm, most of which were inactive.
"Word for word, what the doctor said, he goes, 'Uh, I can maybe make this one work’,” Underwood told Men’s Health last year. “This one?!"
It may sound like an impossible situation — but IVF can surmount even this sort of obstacle.
“Usually, for an IUI insemination, we're looking for about 10 million sperm to be present,” Puetz says. “With only having four or five sperm, IVF is definitely going to be a more effective treatment, because in IVF our embryologists are able to isolate a single sperm and perfectly inseminate a single egg. They're able to fully assist that maneuver, versus in IUI, where, even though we put the sperm into the uterus, the sperm still has to travel up the fallopian tube, meet the egg, and burrow through the egg’s outer layer to get to the egg and fertilize it.
"If you have a lower sperm count, IVF is going to be a better route to go, versus IUI,” Puetz summarizes.

There are other reasons why one approach might work better for a queer family’s unique needs than the other, including finances and family planning.
“The cost is typically going to be much lower in an IUI procedure versus IVF,” Puetz points out, “but your long-term family-building abilities are greater in IVF, because in once cycle of IVF you have the potential to hopefully make several embryos and capture your fertility at that time.” Ordinarily, IVF can generate a number of viable embryos all at the same time — and while only one will be implanted, the others can be saved through cryogenic preservation, allowing for a second, third, or more children in later years. The freezing of embryos — or of sperm and ova — acts as a hedge against time or other subsequent medical considerations that might impact an individual’s fertility.
“Age is one of the biggest factors that we're working against,” Puetz adds. “IVF gives you the ability to basically capture the quality of your egg at that that time, versus as we age, when we're potentially going to see impact on eggs.”
Though fertility preservation acts as a kind of time machine for the quality of a person’s genetic material, the benefits remain tangible in the here and now. For two individuals with sperm, “if you're doing IVF, you would have the ability to select an egg donor who maybe has certain characteristics that you're looking for, and then a separate person as your gestational carrier,” Puetz says. “Maybe what you're looking for in an egg donor is going to be very difficult to find in both a gestational carrier and an egg donor. IVF allows you to separate those two pieces. If you are looking for an egg donor who is going to do inseminations, you want to match with their entire genetic profile, as well as their ability to carry a pregnancy.”
Moreover, “Usually with gestational carriers, we are looking for a history of successful pregnancies,” Puetz goes on to explain. “In egg donors, you don't necessarily see that; a lot of egg donors maybe haven't had children yet.”

Then there’s the possibility of deepening an intimate bond with a life partner through what’s called reciprocal IVF — an approach that allows two people with wombs to carry pregnancies achieved with the ova of their partners. “That is a beautiful option, so that both parties feel like they are involved in in the pregnancy,” Puetz says.
Then too, one partner with a womb might also choose to carry an embryo created from the other partner’s womb simply because the egg donor can’t, or prefers not to, carry the pregnancy. “That would be someone who wouldn't be a good candidate for IUI,” Puetz points out. “But if they're open to being genetically related to the child, they might still be a candidate for IVF.”
Most families would probably space the arrival of children a few years apart, which means that building a family with several children might take a decade or more. Here, too, fertility preservation might play a role. “You see lots of situations also that have to do with that age factor that we talked about,” Puetz notes. “Maybe we had the first baby using IUI when we were in our early thirties. Now we're ready for second baby, and we're in those late thirties, and we're thinking maybe, down the line, we're going to want baby number three, right? What’s a time we’ll be ready for baby number three? We might be into our forties at that point.”
It's in a situation like this that a couple might switch things up, going with IVF where they once used IUI.
“The thought is, ‘Well, if we do IVF, then we can freeze embryos or eggs, at that point in time’,” Puetz explains. “So, it's a really big thing for family planning, fertility preservation, and giving people a chance to make that decision and not have to make it in that moment.”
Kilian Melloy serves as EDGE Media Network's Associate Arts Editor and Staff Contributor. His professional memberships include the National Lesbian & Gay Journalists Association, the Boston Online Film Critics Association, The Gay and Lesbian Entertainment Critics Association, and the Boston Theater Critics Association's Elliot Norton Awards Committee.